(NB updating/working text which was probably 10-15 years)
Evidence in clinical medicine practice – giving what info about what for whom to what purpose?
Is really reductionstic and nomothetic based evidence relevant and interested for clinicians who meet real people living in a real world? Of course we could say that we do not have systems integrating knowledge, methodology and money to meet real worlds demands but then the question emerges; is man for medical science or the reversed?`
The development of useful information for clinical work is addressed more and more while evidence based medicine usually neglect individual (ideographic) perspective and thereby to not give much info about Hans and Greta in their real life and health situation.
It is really about time to request scientific work not only of normative interests (which of course has its normative importance) but hard work to really address and try to increase understanding of real people in real life, what we call biopsychosocial-cultural medicine perspective/paradigm (based on http://www.newriver.edu/images/stories/library/Stennett_Psychology_Articles/Need%20for%20a%20New%20Medical%20Model%20-%20A%20Challenge%20for%20Biomedicine.pdf work).
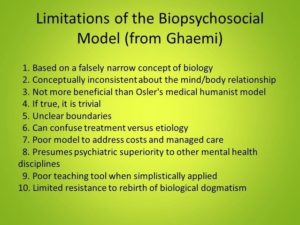
E.g. on critics of the biopsychosocial model is below from https://www.psychologytoday.com/blog/theory-knowledge/201510/the-biopsychosocial-model-and-its-limitations
Here is a summary list of critiques of the BPS model from Ghaemi (2011).
 (my own critics – working text – at http://biopsychosocialmedicine.com/?page_id=32) – 10 Questions | Biopsychosocial Medicine
(my own critics – working text – at http://biopsychosocialmedicine.com/?page_id=32) – 10 Questions | Biopsychosocial Medicine
I will not discuss the above critics right now but move on and ask a question, which is
-> Although most clinicians during last thousands of years have observed that individuals vary in most respects within and between as well as over situations and time, a priority for development of a biopsychosocial-cultural approach has not been substantial developed – knowledge-empirical-educational-practical based. Any objections? Instead has the western medicine development focused on a reductionist based platform/paradigm with normative focus which cannot address real world. Why? Medicine concerns patients – suffering and needing proper examination and treatment but also a prevention perspective is needed as well.
To argue “it is not well developed” requires the question “way not”! Wrong paradigm? Impossible to address (which is true for a reductionstic paradigm) ….?
If not a considerable priority for a lifestyle relevant focus on lifestyle related diseases and mental problems we cannot accuse biopsychosocial medicine to be limited – we could say that it has been a limited interests and limited priority for its development as well as limited need to substantially develop the field while lifestyle related diseases are not to be priority for societies and health care systems!
Some would perhaps argue that the development of evidenced based practice is satisfactory – or?
Our way – out of a biopsychosocial stress medicine paradigm – to address the lack of satisfactory evidenced based knowledge-empirical-practical clinical work is to used IBED, Individual Biopsychosocial Evidenced based Documentation which also give dynamic evidenced information real time. This can be done both at examination as well as during interventions and posttests!
Some text to be more proper included than below;
Kazdin
Below from http://www.healthparc.com/Documents/Kazdin,%202008.pdf I do some comment after BvS-> underlined in Kazdins text.
“Research can do more to identify moderators of treatment and how they make a difference (i.e., across one treatment or all treatments BvS-> as well as relevance concerning variations between and within individuals over situations and time – see e.g. R.S: Lazarus as well as Zimbardo below) and to report these results so that clinicians can make better decisions. I mentioned qualitative research as a third priority because it provides a methodology in which rigor and clinical relevance unite.
I recognize that accredited programs in psychology may not even mention qualitative research yet may offer courses on the subject. I have taught research methodology at the graduate level at three universities. Within the quantitative/null hypothesis tradition there is so much to teach. Ongoing advances must constantly be added to the canon to prepare students competently. There is little time to train in other traditions (e.g., qualitative research, single-case experimental designs) given the scope of courses required, perhaps especially so for clinical and counseling psychology students, who have additional courses and experiences required for state licensing. Still, it is worth mentioning here because qualitative research allows intensive study of individuals in a scientifically rigorous way and for these reasons bridges the research–practice divide. Shifts in emphases in clinical practice were also suggested.
Monitoring treatment with systematic assessment was the first suggestion. Using an EBT, whether integrated with experience, judgment, and contextual considerations or not, of course, does not guarantee a positive treatment outcome. This is a major reason why the patient’s progress should be monitored in a systematic way if at all possible. Our many unique contributions as psychologists include remarkable literatures on cognitive heuristics, memory, and perception that teach us why we need such tools. Research on measurement has provided reliable and valid tools that can be used in clinical and other applied settings to benefit directly the people we serve. Research on psychological treatments conveys what we can do to increase the likelihood of producing therapeutic change. There is no other discipline that can claim any of this or that is in such a position to provide empirically supported treatment and assessment.
Finally, assessment in the context of patient care will overcome what I consider to be a very regrettable loss of accumulated knowledge from clinical practice. We do not benefit as a field from the accumulated practice of clinicians, with the rare exception of those whose groundbreaking treatments may spawn empirical research. For the rest of us, there is a potentially rich data set lost when our practices end. We do not need the clinician to become a researcher any more than we want the researcher to become a practitioner. Both the clinician and the researcher can mine the data for practical and scientific questions”.
BvS-> Kazdin´s argument above can be used as a platform for IBED, Integrated Biopsychosocial Evidenced base Documentation, where www.ipbm.se (integrated psychophysiological behavioral medicine) represent and point of departure). What useful info does IPBM add? As we focus on autonomic nervous system dynamic behaviors we can test and observe individuals´ dynamic capacity to control their own ANS-behaviors. As ANS function as a common denominator associated direct and indirect as well with most lifestyle and stress related diseases and mental dysfunctions it does have important relevance.
When we furthermore can identify interplay between psychological and physiological behaviors we can gradually coach via real time and not real time biofeedback to increased their capacity gradually to – over time construe a habit based on operational conditioning (biologic learning – cope with life events more effectively.
IBED is an IPBM-based single case design which can be the point of departure also for moving up to normative levels.
Folkman, Lazarus et al
https://www.researchgate.net/profile/Christine_Schetter/publication/232485259_Dynamics_of_a_Stressful_Encounter_Cognitive_Appraisal_Coping_and_Encounter_Outcomes/links/09e414ff215b3ebb95000000/Dynamics-of-a-Stressful-Encounter-Cognitive-Appraisal-Coping-and-Encounter-Outcomes.pdf
… “Finally, the results of this study support the importance of intraindividual analyses as a method of understanding the relations between the contextual features of specific stressful encounters and coping processes and the relations between these variables and short-term encounter outcomes. However, an understanding of the relations between coping processes and the long-termed adaptational outcomes, which is a major goal of stress and coping research, also requires an interindividual approach in which people are compared with each other with respect to the ways they cope with diverse stressful encounters over time (e.g. Folkman et al., 1986). Both intraindividual and interindividual approaches are needed to understand coping processes and the mechanisms through which they come to affect people´s wellbeing over the long term”
See also – https://www.ncbi.nlm.nih.gov/pubmed/3712234
Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ.
Abstract: Despite the importance that is attributed to coping as a factor in psychological and somatic health outcomes, little is known about actual coping processes, the variables that influence them, and their relation to the outcomes of the stressful encounters people experience in their day-to-day lives. This study uses an intraindividual analysis of the interrelations among primary appraisal (what was at stake in the encounter), secondary appraisal (coping options), eight forms of problem- and emotion-focused coping, and encounter outcomes in a sample of community-residing adults. Coping was strongly related to cognitive appraisal; the forms of coping that were used varied depending on what was at stake and the options for coping. Coping was also differentially related to satisfactory and unsatisfactory encounter outcomes. The findings clarify the functional relations among appraisal and coping variables and the outcomes of stressful encounters.
(from NIH notes – Investigated the functional relations among cognitive appraisal and coping processes and their short-term outcomes within stressful encounters. The authors used an intraindividual analysis of the interrelations among primary appraisal (what was at stake in the encounter), secondary appraisal (coping options), 8 forms of problem- and emotion-focused coping, and encounter outcomes in a sample of 85 married couples (females aged 35–45 yrs and males aged 26–54 yrs). Findings show that coping was strongly related to cognitive appraisal; the forms of coping that were used varied depending on what was at stake and the options for coping. Coping was also differentially related to satisfactory and unsatisfactory encounter outcomes. Findings clarify the functional relations among appraisal and coping variables and the outcomes of stressful encounters. (47 ref) (PsycINFO Database Record (c) 2016 APA, all rights reserved)
See also http://web.ba.ntu.edu.tw/luolu/COPING%20CONSISTENCY%20AND%20EMOTIONAL%20OUTCOME.pdf
https://cds.psych.ucla.edu/pubs/1986%20FolkmanLazarus_Dynamics%20of%20a.pdf
-> http://psycnet.apa.org/psycinfo/1986-21910-001
Zimbardo
From http://www.thetimeparadox.com/wp-content/uploads/2012/09/1999PuttingTimeinPerspective.pdf
Putting Time in Perspective: A Valid, Reliable Individual-Differences Metric
Philip G. Zimbardo and John N. Boyd, Stanford University
Abstract: Time perspective (TP), a fundamental dimension in the construction of psychological time, emerges from cognitive processes partitioning human experience into past, present, and future temporal frames. The authors’ research program proposes that TP is a pervasive and powerful yet largely unrecognized influence on much human behavior. Although TP variations are learned and modified by a variety of personal, social, and institutional influences, TP also functions as an individual-differences variable. Reported is a new measure assessing personal variations in TP profiles and specific TP “biases.” The 5 factors of the Zimbardo Time Perspective Inventory were established through exploratory and confirmatory factor analyses and demonstrate acceptable internal and test—retest reliability. Convergent. divergent, discriminant, and predictive validity are shown by correlational and experimental research supplemented by case studies.
Some comments
1. First cognitive appraisal need to be expanded to include precognitive appraisal as we understand it out of a evolutionary perspective on human brain development! But this has been an observation done earlier without considering functioning of mammalian and reptilian brain! E,g, Arvid Kappas – http://www.tandfonline.com/doi/abs/10.1080/02699930600616080?scroll=top&needAccess=true&journalCode=pcem20 writes; “In 1960, Magda Arnold defined the appraisal construct as being causal to emotion. Appraisal, according to her, refers to a direct, immediate, and intuitive process that does not initially require recognition of the object that is being appraised. It is based on phylogenetically ancient subcortical brain structures. In addition, Arnold proposed the existence of a related conscious process, also referred to as appraisal, that interacts with the direct appraisal and is responsible for a differentiation of emotional states. This theory was revolutionary and is still to be considered modern because it already comprised much of what is currently hypothesised to be causal for emotion. However, Lazarus, who initially believed that conscious aspects of appraisal are more important than implicit and unaware appraisals, coined the term cognitive appraisals and popularised this notion widely. In opposition to what he perceived as a prevailing emphasis on higher cognitive processes in emotion theory, Zajonc (1980 Zajonc, R. B. 1980. Feeling and thinking: Preferences need no inferences. American Psychologist, 39: 151–75. [Google Scholar]) argued that emotion elicitation does not depend on conscious cognition. I argue that Arnold’s theory is in fact completely consistent with Zajonc’s view and data. The concept of appraisal should be discussed in relation to Arnold’s original intention, because it provides not only the basis of an integrated view of multiple levels of emotional processing, encompassing views espoused by Zajonc and by Lazarus, but may guide current and future research on multiple levels of processing in the elicitation of emotions”.
BvS-> Although most scientists today interested in human brain functions related to clinical medicine/psychology/psychiatry realize that most of human brain information processing – including autonomic nervous-, immune systems as well as emotional processes – occurs at not conscious levels, of which we unfortunately understand quite little of but can observe effects of, it is such complex that we do have little to offer concerning examination, treatment and evaluations. As a clinicians you must make decisions (at best in cooperation with your patients, which is a living human not to be neglected but more reasons than that cooperation is a prerequisite in most treatments. This means that it is not only an educational matter but also a cultural one including basic internalized attitudes, values, stance and paradigm as well as world hypothesis (Stephen Pepper, 1942).
2. Critics and controversies about a sound medical paradigms of clinical relevance has been not well met which has prevented a sound development of a systems integrated multidisciplinary biopsychosocial platform for medical research. Some argue this is due to profits interests, above all pharmacological interests, which might even be escalated last 1-30 years, e.g. the epidemic promoted development of ADHD (see e.g. Allan Francis publications). This is not acceptable and should be subjected to independent investigations! This concerns not only what is relevant today but also how this even has been possible to be controlled as critics argue! Furthermore, how will this be treated in the future. Much economical investment may be directed to find new ways to bring status que ahead!
3. As systems integrated biopsychosocial-cultural medical paradigm is even hardly started there are huge challenges at all levels; knowledge – methodological – practical – educational – interactive communicated based as well as structural and economical. When patients are educated in terms of “patient as an educated, relevant competent resource in her/his own rehabilitation” (or prevention activities) probably individuals and societies will face also economic benefits but the way until this goal is probably long requiring also vast educational efforts of health care systems workers! Here is a long termed challenge for the whole societies where politicians are expected to take the lead!
Summarizing; While an effective biopsychosocial medicine is not yet substantially developed is not difficult to understand for those sharing others and my own arguments above just because it can be argued “it is not possible to develop related to …. ” but as discussed above this is not acceptable. Keeping a reducitonstic point of departure is not possible although this can be regarded as almost hardware in our scientific and educational paradigm. This means that we need to start, not at “0” but at “-100” when we relearn basic we take for granted!
How can this be done while at the same time provide as effective health care services as possible? There is a way I see but I will wait to discuss this until I see an interests as well as others ideas …
More within some time ….
Below I will briefly describe our approach …
